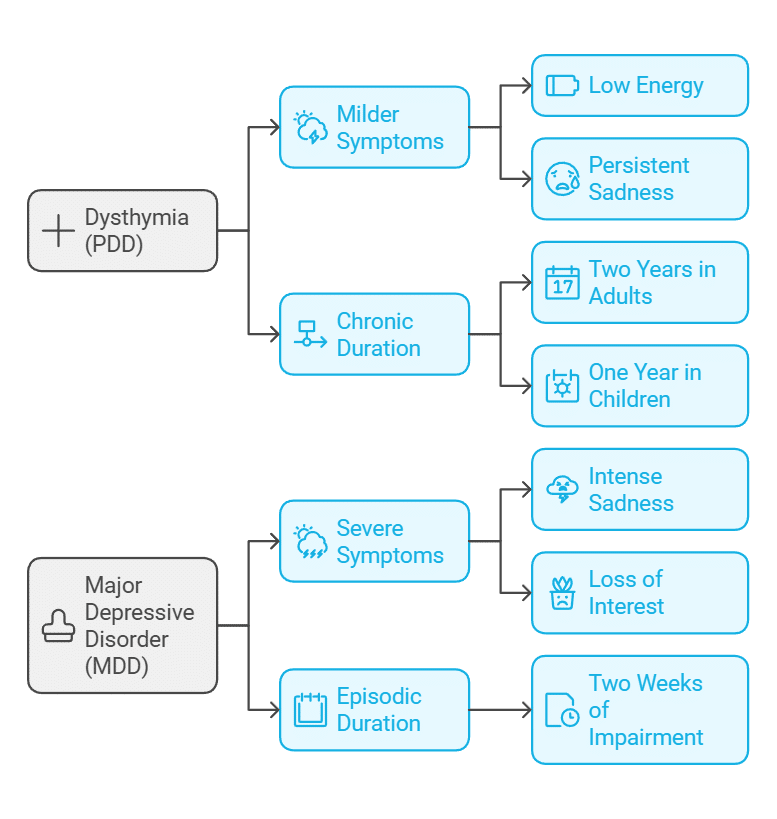
Mood disorders are complex and multifaceted, often presenting in ways that significantly impact an individual’s emotional well-being and daily life. Two of the most commonly discussed forms of depression are Dysthymia (Persistent Depressive Disorder) and Major Depressive Disorder (MDD). While both conditions are characterized by persistent low mood and emotional distress, they differ in severity, duration, and overall impact on quality of life. This blog post explores the key differences between these two disorders, focusing on definitions, symptoms, diagnostic criteria, treatment approaches, and their long-term effects.
Definitions and Symptoms
What is Dysthymia (Persistent Depressive Disorder)?
Dysthymia, now formally known as Persistent Depressive Disorder (PDD), is a chronic form of depression that persists for at least two years in adults or one year in children and adolescents. Unlike major depression, dysthymia typically involves milder symptoms that are consistent over time.
Symptoms of Dysthymia:
- Low energy or fatigue
- Persistent feelings of sadness or hopelessness
- Low self-esteem
- Difficulty concentrating or making decisions
- Changes in appetite (either overeating or under-eating)
- Sleep disturbances (insomnia or hypersomnia)
- Individuals with dysthymia often describe feeling as though they are merely going through the motions of life, with their condition becoming a “new normal.”
What is Major Depressive Disorder (MDD)?
Major Depressive Disorder is a more intense and episodic form of depression, marked by a distinct period of at least two weeks where symptoms interfere significantly with daily functioning. MDD often appears suddenly and may be triggered by life events, though it can also develop without a clear cause.
Symptoms of MDD:
- Intense feelings of sadness, emptiness, or hopelessness
- Loss of interest or pleasure in activities once enjoyed
- Significant changes in appetite and weight
- Sleep disturbances (insomnia or excessive sleeping)
- Feelings of worthlessness or excessive guilt
- Difficulty concentrating or indecisiveness
- Recurrent thoughts of death or suicide
While MDD is typically more severe, dysthymia’s chronic nature can lead to comparable challenges over time.
Diagnostic Criteria
Proper diagnosis is crucial for differentiating between dysthymia and major depression. Both disorders are identified using criteria outlined in the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders).
Diagnostic Criteria for Dysthymia:
- Depressed mood for most of the day, for more days than not, lasting at least two years (one year for children/adolescents).
- Presence of at least two of the following symptoms:
- Poor appetite or overeating
- Insomnia or hypersomnia
- Low energy or fatigue
- Low self-esteem
- Poor concentration or difficulty making decisions
- Feelings of hopelessness
- Symptoms must cause clinically significant distress or impairment in social, occupational, or other areas of functioning.
- The individual must not have been without symptoms for more than two consecutive months during the two-year period.
Diagnostic Criteria for Major Depressive Disorder:
- Presence of five or more of the following symptoms during the same two-week period, with at least one being either depressed mood or loss of interest/pleasure:
- Depressed mood most of the day, nearly every day
- Markedly diminished interest or pleasure in most activities
- Significant weight loss or gain, or changes in appetite
- Insomnia or hypersomnia
- Psychomotor agitation or retardation
- Fatigue or loss of energy
- Feelings of worthlessness or excessive guilt
- Difficulty concentrating or indecisiveness
- Recurrent thoughts of death or suicide
- Symptoms must cause significant distress or impairment in daily life.
- Episodes are not attributable to substance use or another medical condition.
While dysthymia requires chronicity, MDD is diagnosed based on the severity and duration of symptoms during specific episodes.
Treatment Approaches
Both dysthymia and major depression require tailored treatment plans that address the unique challenges of each condition. A combination of psychotherapy, medication, and lifestyle changes is often the most effective approach.
Treating Dysthymia
The chronic nature of dysthymia necessitates long-term treatment strategies that focus on improving baseline mood and preventing relapse. Common treatments include:
- Psychotherapy: Cognitive Behavioral Therapy (CBT) to challenge negative thought patterns.
Interpersonal Therapy (IPT) to improve social functioning. - Medications: Selective Serotonin Reuptake Inhibitors (SSRIs) like fluoxetine or sertraline.
Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) for persistent symptoms. - Lifestyle Modifications: Regular physical activity and mindfulness practices to stabilize mood.
Building strong support systems to combat feelings of isolation.
Treating Major Depressive Disorder
MDD often requires a more intensive, immediate intervention due to the severity of symptoms:
- Psychotherapy
- CBT to address maladaptive thinking and behaviors.
- Dialectical Behavior Therapy (DBT) for emotional regulation.
- Medications:
- SSRIs and SNRIs are first-line treatments.
- Tricyclic antidepressants (TCAs) or monoamine oxidase inhibitors (MAOIs) for treatment-resistant cases.
- Other Interventions:
- Electroconvulsive Therapy (ECT): For severe, treatment-resistant depression.
- Transcranial Magnetic Stimulation (TMS): A non-invasive option for chronic depression.
- Lifestyle Adjustments:
- Encouraging adherence to treatment plans and promoting healthy routines.
The key to effective treatment lies in regular monitoring and adjustments based on the individual’s response.
Long-term Impacts on Quality of Life
Dysthymia
The chronic nature of dysthymia often leads to a pervasive sense of dissatisfaction with life. Individuals may struggle with:
- Reduced Productivity: Chronic fatigue and low motivation can impact career progression.
- Social Challenges: Persistent low mood may result in withdrawal from relationships and social activities.
- Increased Risk of Comorbidities: Anxiety disorders, substance use disorders, and major depression are common co-occurring conditions.
With proper management, individuals with dysthymia can achieve improved quality of life, but the condition often requires sustained effort and support.
Major Depressive Disorder
The episodic nature of MDD means periods of remission may alternate with relapses, significantly disrupting life. Long-term effects can include:
- Impact on Relationships: Intense depressive episodes can strain personal and professional relationships.
- Health Risks: Untreated MDD is linked to higher rates of chronic illnesses, such as cardiovascular disease.
- Increased Risk of Suicide: MDD carries a higher risk of suicidal thoughts and behaviors, underscoring the need for timely intervention.
With effective treatment and coping strategies, individuals can achieve remission and lead fulfilling lives, but vigilance is necessary to prevent recurrence.
While dysthymia and major depressive disorder share common symptoms, their differences in duration, severity, and treatment needs are crucial for understanding and managing each condition. By recognizing the distinctions, individuals and healthcare providers can work together to create personalized treatment plans that address specific challenges. At Amavi Integrative Mental Wellness, we are dedicated to providing comprehensive care for mood disorders, empowering individuals to achieve emotional balance and improved well-being. If you or a loved one is experiencing symptoms of depression, reach out today to start your journey toward recovery.