Anxiety disorders rarely exist in isolation. Many individuals with anxiety also experience co-occurring mental health conditions, which can complicate diagnosis and treatment. These coexisting disorders may exacerbate symptoms, making it essential to understand how they interact and how to manage them effectively. This blog explores common co-occurring conditions like depression and OCD, the challenges they pose to diagnosis, and the benefits of integrated treatment approaches.
1. Overview of Common Co-occurring Conditions Like Depression and OCD
Anxiety often overlaps with other mental health disorders, creating a complex interplay of symptoms that can impact daily functioning. Understanding these conditions and their relationship to anxiety is crucial for effective care.
Depression
Depression is one of the most common co-occurring conditions with anxiety. Research indicates that nearly 50% of individuals diagnosed with an anxiety disorder also experience symptoms of depression. While anxiety involves heightened worry and fear, depression is characterized by persistent sadness, loss of interest, and feelings of hopelessness. The combination of these disorders can lead to a cycle where anxiety amplifies depressive symptoms, and vice versa. For example, excessive worry about the future (a hallmark of anxiety) may lead to feelings of helplessness, contributing to depression.
Obsessive-Compulsive Disorder (OCD)
OCD is another condition that frequently co-occurs with anxiety. Individuals with OCD experience intrusive thoughts (obsessions) and feel compelled to perform repetitive behaviors (compulsions) to alleviate their distress. Anxiety often underpins these compulsions, as individuals feel an overwhelming need to prevent perceived harm or discomfort. For instance, someone with contamination fears may experience intense anxiety about germs, leading to excessive handwashing.
Post-Traumatic Stress Disorder (PTSD)
PTSD shares significant overlap with anxiety disorders, particularly generalized anxiety disorder (GAD) and panic disorder. PTSD arises after experiencing or witnessing a traumatic event and includes symptoms like flashbacks, hypervigilance, and avoidance behaviors. Anxiety often exacerbates these symptoms, making daily life more challenging for individuals with PTSD.
Substance Use Disorders
Substance use disorders frequently co-occur with anxiety, as some individuals use drugs or alcohol to self-medicate their symptoms. While substances may provide temporary relief, they often worsen anxiety over time and create additional challenges, such as dependency and withdrawal symptoms.
Other Related Conditions
- Social Anxiety Disorder and Avoidant Personality Disorder: These conditions involve intense fear of social judgment, leading to avoidance of social situations.
- Eating Disorders: Conditions like anorexia nervosa and bulimia can coexist with anxiety, as individuals may experience extreme worry about body image or control.
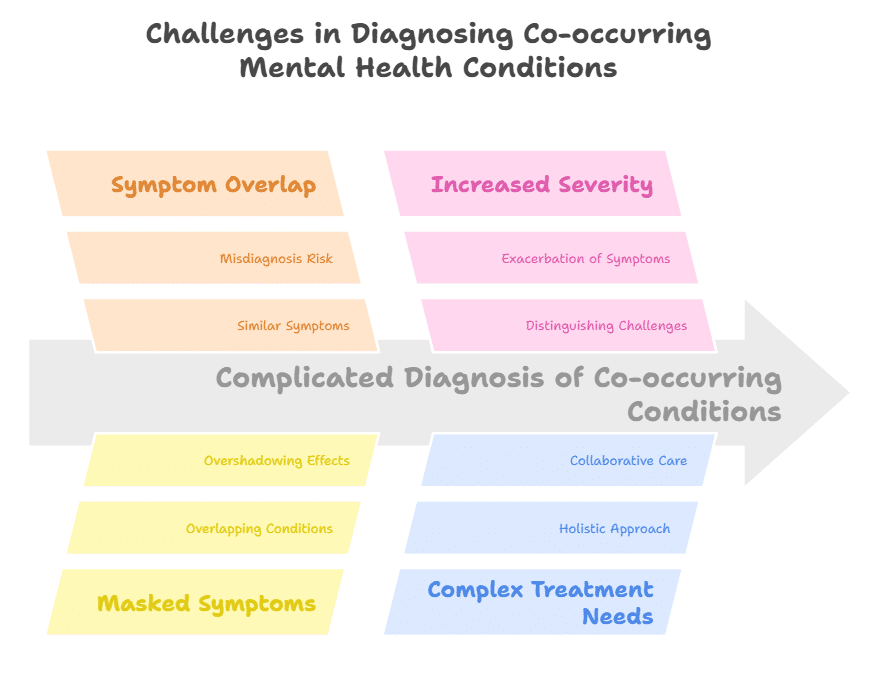
2. How Co-occurring Conditions Complicate Diagnosis
The presence of multiple mental health conditions can blur the lines between diagnoses, making it challenging for clinicians to identify and address the root causes of symptoms.
Symptom Overlap
Many symptoms of anxiety overlap with those of other disorders. For instance, both anxiety and depression can involve fatigue, irritability, and difficulty concentrating. This overlap can lead to misdiagnosis or underdiagnosis of one condition. Similarly, individuals with OCD may exhibit behaviors that resemble those of anxiety or depression, such as avoidance or lack of motivation.
Masked Symptoms
In some cases, the symptoms of one condition may mask or overshadow those of another. For example, someone with severe depression may appear apathetic or withdrawn, making it harder to recognize their underlying anxiety. Conversely, individuals with substance use disorders may attribute their anxiety symptoms to withdrawal, delaying appropriate diagnosis and treatment.
Increased Severity of Symptoms
Co-occurring conditions often exacerbate each other, leading to more severe and debilitating symptoms. For example, individuals with both PTSD and anxiety may experience heightened hypervigilance and panic attacks, making it harder to distinguish between the two disorders. This interplay can complicate the diagnostic process and require a more nuanced evaluation.
Complex Treatment Needs
When multiple conditions are present, treatment plans must address all underlying issues, not just the most apparent symptoms. This complexity often requires collaboration among various healthcare professionals and a holistic approach to care.
3. Integrated Treatment Approaches
Integrated treatment approaches are essential for addressing the interconnected nature of co-occurring conditions. These strategies focus on treating the whole person rather than isolated symptoms, improving outcomes and quality of life.
Comprehensive Assessment
The first step in integrated care is a thorough assessment to identify all co-occurring conditions. This includes:
- Detailed medical and psychiatric history to uncover potential risk factors.
- Standardized screening tools, such as the Generalized Anxiety Disorder-7 (GAD-7) scale or the Patient Health Questionnaire-9 (PHQ-9), to assess anxiety and depression symptoms.
- Evaluations for substance use, trauma history, or other relevant conditions.
By understanding the full spectrum of a patient’s mental health, clinicians can develop a targeted treatment plan.
Evidence-Based Therapies
Cognitive Behavioral Therapy (CBT) is a cornerstone of integrated treatment, as it is effective for both anxiety and co-occurring conditions like depression and OCD. CBT helps individuals identify and challenge negative thought patterns, develop coping strategies, and address specific triggers. For OCD, Exposure and Response Prevention (ERP)—a specialized form of CBT—helps reduce compulsions and manage intrusive thoughts.
Other therapeutic approaches include:
- Trauma-Focused CBT: Tailored for individuals with PTSD and anxiety, this therapy addresses trauma-related symptoms while building resilience.
- Dialectical Behavior Therapy (DBT): Effective for individuals with anxiety and co-occurring personality disorders, DBT teaches skills for emotion regulation and interpersonal effectiveness.
Medication Management
Medications, such as selective serotonin reuptake inhibitors (SSRIs), are commonly prescribed for anxiety, depression, and OCD. In some cases, additional medications, like mood stabilizers or antipsychotics, may be necessary to address co-occurring conditions. A psychiatrist can tailor medication regimens to an individual’s unique needs, ensuring that all symptoms are adequately managed.
Lifestyle Interventions
Lifestyle changes play a vital role in integrated care. Regular exercise, a balanced diet, and adequate sleep improve overall mental health and help regulate mood and anxiety. Mindfulness practices, such as meditation and yoga, can further enhance emotional well-being by reducing stress and promoting relaxation.
Collaborative Care Models
Integrated treatment often involves collaboration among multiple healthcare providers, including therapists, psychiatrists, primary care physicians, and substance abuse counselors. This team-based approach ensures that all aspects of a patient’s mental health are addressed cohesively.
A Holistic Path to Mental Wellness
Co-occurring conditions and anxiety present unique challenges, but with the right approach, they are manageable. Understanding the interplay between anxiety and related disorders, recognizing how they complicate diagnosis, and adopting integrated treatment strategies are essential for effective care.
If you or a loved one is struggling with anxiety and co-occurring conditions, know that help is available. Contact Amavi Integrative Mental Wellness for personalized care and you can find relief and regain control over your mental health, paving the way for a brighter and more balanced future.