Obsessive-Compulsive Disorder (OCD) often does not exist in isolation. Many individuals with OCD experience other mental health conditions, known as comorbid or co-occurring disorders, which can complicate diagnosis and treatment. These overlapping conditions may intensify OCD symptoms, impact daily functioning, and pose unique challenges for clinicians and individuals seeking help. In this blog, we’ll explore common comorbid conditions, the complexities they add to diagnosis and treatment, and the benefits of integrated treatment plans that address the whole person.
1. Exploring Common Comorbid Conditions Like Anxiety and Depression
Research shows that over 50% of individuals with OCD have at least one additional mental health condition, making it critical to understand these comorbidities for effective treatment. Anxiety disorders are among the most common co-occurring conditions with OCD. These disorders, including generalized anxiety disorder (GAD) and social anxiety disorder (SAD), share similar mechanisms, such as heightened stress responses and cognitive distortions. GAD involves persistent, excessive worry about various aspects of life, which can fuel compulsive behaviors as coping mechanisms. Meanwhile, SAD can exacerbate OCD symptoms when compulsions, such as handwashing or checking, become noticeable in social settings, leading to heightened fear of judgment or embarrassment.
Depression is another frequent comorbidity, often arising from the chronic stress and frustration associated with managing OCD. The cyclical nature of OCD—where compulsions provide only temporary relief from obsessions—can lead to feelings of hopelessness and despair. These individuals may withdraw socially, experience low energy, and struggle with motivation, further complicating their ability to engage in treatment.
Body dysmorphic disorder (BDD), a condition within the OCD spectrum, involves obsessive preoccupation with perceived flaws in one’s appearance. This condition shares characteristics with OCD, such as intrusive thoughts and compulsive behaviors aimed at alleviating distress. Similarly, tic disorders, including Tourette syndrome, often co-occur with OCD, particularly in children and adolescents. The overlapping neurological pathways of tics and compulsions can make diagnosis and treatment more challenging.
Other common co-occurring disorders include post-traumatic stress disorder (PTSD) and substance use disorders. Traumatic experiences can intensify OCD symptoms or lead to compulsions aimed at avoiding trauma-related triggers. Some individuals may turn to drugs or alcohol to self-medicate their OCD-related anxiety, further complicating their overall mental health and treatment outcomes.
2. How Co-occurring Disorders Complicate OCD Diagnosis and Treatment
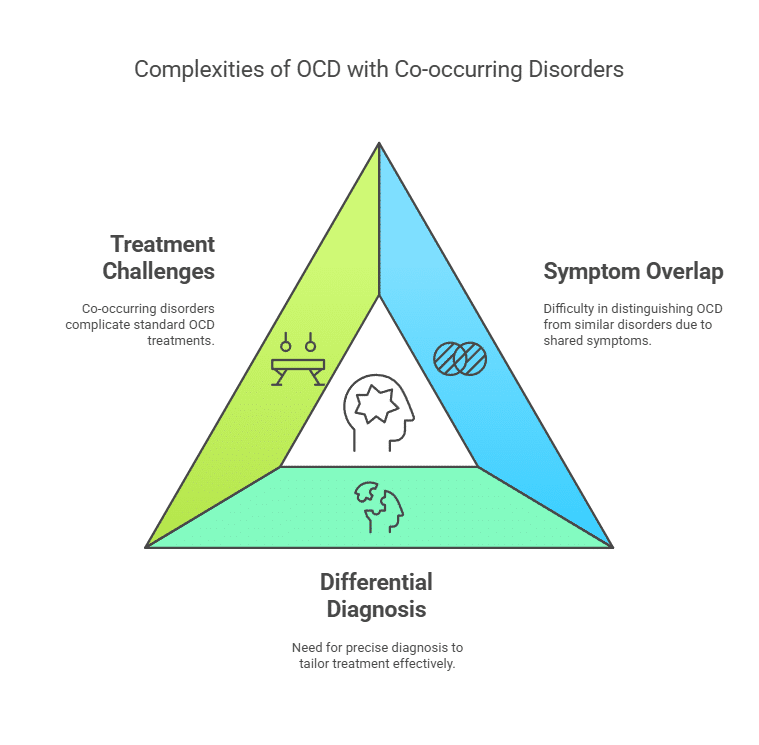
When OCD coexists with other mental health conditions, diagnosis and treatment become more complex. The overlapping symptoms of these disorders often blur diagnostic boundaries, making it challenging for clinicians to accurately identify and prioritize conditions.
One major challenge is the significant symptom overlap between OCD and other disorders. For instance, excessive worry and avoidance behaviors are common in both anxiety disorders and OCD. A person with OCD may avoid social gatherings to prevent triggers for their compulsions, while someone with social anxiety disorder may avoid them due to fear of judgment. These similarities can make it difficult to distinguish one condition from another. Additionally, a co-occurring disorder may mask or overshadow OCD symptoms. For example, severe depression may dominate the clinical presentation, causing clinicians to miss underlying obsessions and compulsions.
The need for differential diagnosis further complicates the process. Clinicians must distinguish OCD from related conditions such as BDD or hoarding disorder, as each requires a tailored treatment approach. Misdiagnosis or incomplete diagnosis can delay effective interventions and worsen the individual’s condition.
Co-occurring disorders also impact treatment in several ways. The presence of multiple conditions often reduces the effectiveness of standard OCD treatments. For example, depression may hinder an individual’s motivation to engage in cognitive-behavioral therapy (CBT), while substance use can interfere with the efficacy of medications like selective serotonin reuptake inhibitors (SSRIs). The severity of symptoms also increases when disorders coexist, leading to greater distress and impairment. This intensifies the need for a comprehensive and carefully balanced treatment approach.
3. Benefits of Integrated Treatment Plans for Holistic Care
To effectively manage OCD and its co-occurring conditions, a holistic, integrated approach is essential. These treatment plans address the interconnected nature of mental health conditions and provide comprehensive care that focuses on the individual as a whole.
A thorough assessment is the foundation of an integrated treatment approach. Multidisciplinary teams conduct evaluations to identify all existing conditions and understand how they interact and influence one another. This process ensures that no condition is overlooked and helps clinicians prioritize treatment goals based on the individual’s unique needs.
Integrated treatment plans often combine multiple therapeutic modalities to address the spectrum of symptoms. Cognitive-behavioral therapy (CBT), particularly exposure and response prevention (ERP), remains the cornerstone of OCD treatment. CBT’s structured approach helps individuals confront their obsessions without resorting to compulsions, while cognitive restructuring addresses symptoms of anxiety and depression. Acceptance and commitment therapy (ACT) complements CBT by encouraging individuals to accept intrusive thoughts rather than fighting them, making it particularly effective for managing both OCD and emotional distress.
Medication management is another critical component of integrated care. SSRIs are commonly prescribed for OCD, anxiety, and depression, with augmentation strategies used for treatment-resistant cases. For instance, combining SSRIs with atypical antipsychotics may help individuals with severe OCD symptoms achieve better outcomes.
Lifestyle interventions further enhance the effectiveness of integrated treatment plans. Regular exercise, a balanced diet, and adequate sleep support overall mental health and improve emotional resilience. Mindfulness meditation and stress management techniques can help individuals reduce the impact of anxiety and enhance their ability to cope with OCD-related challenges.
A multidisciplinary team often delivers holistic care, involving psychiatrists for medication management, therapists for evidence-based therapies, and social workers or case managers for practical support and access to community resources. Family therapists may also be included to involve loved ones in the treatment process, particularly when addressing conditions like OCD and depression.
The Path to Comprehensive Mental Health Care
OCD and its co-occurring disorders present unique challenges that require thoughtful, integrated treatment strategies. By addressing the root causes of symptoms, prioritizing comprehensive assessments, and combining therapy, medication, and lifestyle changes, individuals with OCD and comorbid conditions can achieve significant improvements in their quality of life.
Holistic treatment plans that address the interconnected nature of these conditions empower individuals to regain control over their mental health and foster long-term recovery. If you or someone you love is struggling with OCD and additional mental health challenges, seeking integrated care from a multidisciplinary team at Amavi Integrative Mental Wellness is a crucial step toward a more balanced and fulfilling life.